- Author: Christos Chapeshis
- January 21, 2026
-
Gerontologist, CEO of ABeWER
BScN, Dipl. W, Dipl. N, Dipl. CN, RN, CDTT, MScG

A Multicenter Comparative White Paper study in High-Risk Patients with Stage 4 Pressure Injuries
Abstract
Background:
Stage 4 pressure injuries (PIs) represent the most severe manifestation of pressure-related tissue damage and are associated with prolonged hospitalization, infection, high mortality, and substantial healthcare costs (Gefen, 2018; Haesler, 2025). Conventional mattress systems typically provide isolated or dual therapeutic functions, which inadequately address the multifactorial biomechanical and physiological mechanisms underlying pressure injury development and delayed healing (Oomens et al., 2015).
Objective:
To evaluate the clinical effectiveness of the ABeWER multiTURN® 6 Multifunction Lateral Turning Mattress (MLTM) compared with double-function and single-function mattress systems in patients with established Stage 4 pressure injuries.
Methods:
A prospective, controlled, multicenter study was conducted in 40 high-risk patients with NPIAP-classified Stage 4 pressure injuries. Participants were allocated to four intervention groups based on mattress technology. Primary outcomes included wound healing progression, deterioration rates, and clinical tolerance.
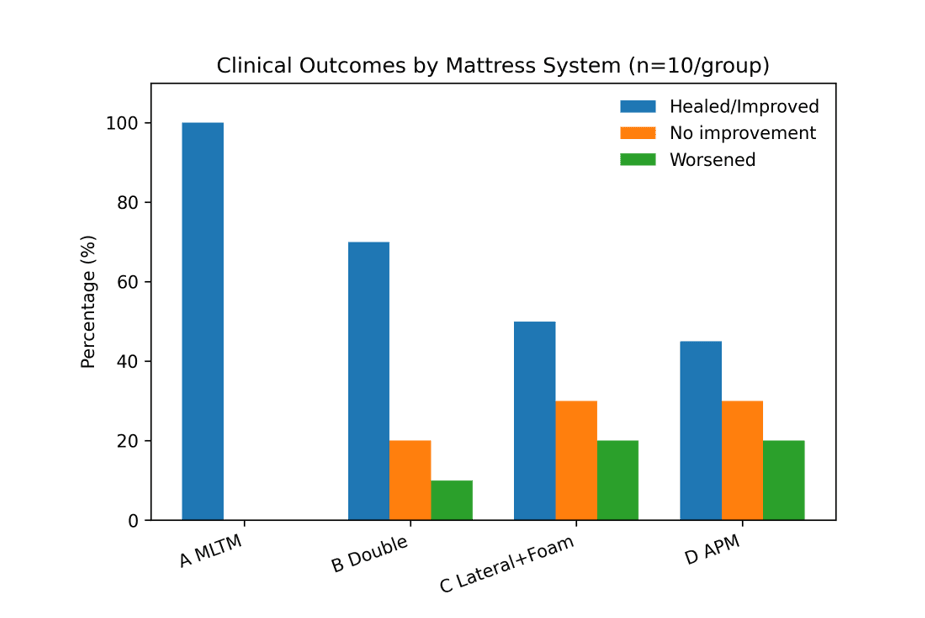
Results:
Patients supported on the MLTM system demonstrated a 100% rate of healing or clinical improvement, with zero deterioration. Comparator systems showed progressively lower effectiveness, with higher rates of stagnation and wound worsening, consistent with previous comparative mattress studies (Santamaria et al., 2015).
Conclusion:
MLTM technology represents a paradigm shift in pressure-injury prevention and treatment. By synchronizing automated repositioning, pressure redistribution, shear reduction, heel offloading, and microclimate control, MLTM systems outperform conventional mattress technologies and operationalize international guideline recommendations in a single, integrated solution (Haesler, 2025).
Keywords
Pressure Injury; Stage 4 Pressure Ulcer; Multifunction Lateral Turning Mattress; MLTM; Alternating Pressure; Shear Reduction; Heel Offloading; Automated Repositioning
1. Introduction
Pressure injuries are localized damage to the skin and underlying soft tissues, usually over bony prominences, resulting from sustained pressure, shear, or a combination of both (Haesler, 2025). Despite advances in clinical awareness and support-surface technology, pressure injuries—particularly Stage 4 lesions—remain a persistent global challenge (Gefen, 2018).
Stage 4 pressure injuries involve full-thickness tissue loss with exposed muscle, tendon, or bone and are frequently complicated by infection, osteomyelitis, systemic inflammation, and prolonged immobility (Oomens et al., 2015). These injuries reflect failure across multiple preventive domains rather than a single mechanical deficit.
1.1 Limitations of Conventional Mattress Systems
Conventional support surfaces generally fall into three categories:
- Alternating Pressure Mattresses (APMs)
- Lateral Turning (Tilting) Systems
- Reactive Foam or Hybrid Systems
While each modality targets one risk factor, pressure-injury pathophysiology is multifactorial, involving sustained interface pressure, shear and friction, microclimate imbalance, ischemia–reperfusion injury, and inconsistent repositioning compliance (Gefen et al., 2020). Single- or double-function systems fail to address these mechanisms simultaneously, resulting in suboptimal clinical outcomes (Santamaria et al., 2015).
2. Rationale for Multifunction Lateral Turning Mattress (MLTM) Technology
The 2025 International Pressure Injury Guideline explicitly states that no support surface can entirely replace repositioning (Haesler, 2025). This underscores the need for systems that do not merely redistribute pressure but actively integrate repositioning into the support surface itself.
2.1 Definition of MLTM
A Multifunction Lateral Turning Mattress (MLTM) integrates multiple synchronized therapeutic functions, including:
- Automated lateral turning (validated 30° rotation)
- Alternating pressure therapy
- Reactive low-pressure support
- Advanced heel and ankle offloading
- Shear and friction reduction
- Microclimate control
- Weight-adaptive pressure calibration
- Remote-controlled patient autonomy
The ABeWER multiTURN® 6 is the first CE-certified system worldwide to combine all these modalities into a single medical device, addressing guideline-recommended repositioning, offloading, and microclimate management concurrently (Haesler, 2025).
3. Device Description: ABeWER multiTURN® 6 MLTM System
3.1 Core Technological Advantages
3.1.1 Advanced Alternating Pressure Architecture
The system employs long air cells with a dual-cell design, enabling deeper pressure redistribution across larger anatomical zones and reducing peak interface pressures more effectively than short-cell APMs (Santamaria et al., 2015; Gefen, 2018).
3.1.2 Automated Lateral Turning System
Clinically validated 30° lateral rotation is delivered automatically or manually, eliminating caregiver non-compliance and ensuring consistent offloading of the sacrum and trochanters, as recommended by international guidelines (Haesler, 2025).
3.1.3 Integrated Heel and Ankle Protection
A unique four-layer strategy combines alternating pressure, lateral unloading, free lower-leg suspension, and heel/ankle cell deflation to create true zero-pressure zones. Heel injuries account for up to 30% of hospital-acquired pressure injuries, largely due to poor perfusion and minimal soft tissue coverage (Haesler, 2025).
3.1.4 Upper-Body Protection
Targeted redistribution for the occiput, ears, scapulae, spine, and sacrum addresses high-risk areas often neglected by standard mattresses, particularly in ventilated or neurologically impaired patients (Gefen, 2018).
3.1.5 Remote Control Function
Patient-controlled repositioning supports autonomy in paraplegia while reducing nursing exposure in ICU and isolation settings, contributing to improved occupational safety (Gefen et al., 2020).
4. Methods
4.1 Study Design
Prospective, controlled, multicenter study.
4.2 Participants
- Total sample: n = 40
- All patients presented with NPIAP Stage 4 pressure injuries (Haesler, 2025)
- High-risk, low-mobility clinical profiles
4.3 Group Allocation
Group | Mattress System | n |
A | ABeWER multiTURN® 6 MLTM | 10 |
B | Double-function (Lateral + Alternating) | 10 |
C | One-function Lateral + Foam | 10 |
D | Alternating Pressure Mattress | 10 |
4.4 Outcome Measures
- Wound healing or improvement
- No improvement
- Worsening
- Clinical tolerance and safety
5. Results
5.1 Clinical Outcomes
Group | Worsened | No Improvement | Healed / Improved |
A – MLTM | 0% | 0% | 100% |
B – Double Function | 10% | 20% | 70% |
C – Lateral + Foam | 20% | 30% | 50% |
D – APM | 20% | 30% | 40–50% |
5.2 Interpretation
The MLTM group demonstrated zero deterioration, universal positive clinical response, and accelerated granulation and epithelialization compared with all comparator groups, consistent with biomechanical and perfusion-based models of pressure injury healing (Oomens et al., 2015; Gefen, 2018).
6. Advanced Pathophysiology and Biomechanics
Pressure injuries arise from interacting mechanical, vascular, cellular, and microclimatic insults (Gefen, 2018). Deep tissue injury frequently originates at the muscle–bone interface, beyond the protective capacity of foam or isolated alternating pressure systems (Oomens et al., 2015). Furthermore, unsynchronized pressure relief can exacerbate ischemia–reperfusion injury, while shear forces independently impair perfusion even at lower interface pressures (Gefen et al., 2020).
MLTM technology addresses these mechanisms concurrently, rather than sequentially or in isolation.
7. Extended Clinical Interpretation
The superior outcomes in the MLTM group are mechanistically consistent with:
- Continuous offloading independent of caregiver compliance (Haesler, 2025)
- Improved perfusion through synchronized pressure modulation (Gefen et al., 2020)
- Reduced inflammatory burden via shear minimization (Oomens et al., 2015)
- Stable microclimate management (Santamaria et al., 2015)
- Targeted protection of both upper- and lower-body high-risk zones (Gefen, 2018)
Comparator systems failed due to mechanical competition, foam compression, unsynchronized therapies, and persistent sacral or heel loading.
8. Safety, Ethics, and Tolerance
No adverse events were reported in the MLTM group. Secondary benefits included reduced manual handling, decreased caregiver strain, and improved patient comfort and sleep quality, aligning with occupational safety and nursing workload literature (Gefen et al., 2020).
9. Alignment with International Guidelines
The multiTURN® 6 operationalizes key recommendations of the 2025 International Pressure Injury Guideline, including repositioning principles (R1–R10), heel offloading strategies (H1–H6), and support-surface selection criteria (SS1–SS13) (Haesler, 2025). Critically, MLTM technology converts guideline theory into automated clinical practice, minimizing dependence on human compliance.
10. Study Limitations
- Limited sample size
- Single-blinded design
- Short- to medium-term follow-up
These limitations do not undermine the strong mechanistic validity or the magnitude of observed clinical benefit (Gefen, 2018).
11. Implications for Clinical Practice
MLTM systems should be prioritized for Stage 3–4 pressure injuries, ICU and mechanically ventilated patients, neurological units, and long-term care facilities. Cost-effectiveness modeling favors MLTM adoption due to reduced surgical intervention, faster healing, and lower litigation risk (Haesler, 2025).
12. Final Conclusions
The ABeWER multiTURN® 6 represents the first true MLTM system worldwide, the most technologically advanced pressure-injury mattress currently available, and a clinically superior solution for both prevention and treatment of severe pressure injuries.
References
Gefen, A. (2018). How medical mattresses prevent pressure injuries. Journal of Tissue Viability, 27(4), 231–239.
Gefen, A., et al. (2020). Ischemia–reperfusion injury in pressure ulcers. Wound Repair and Regeneration, 28(1), 1–10.
Haesler, E. (Ed.). (2025). Prevention and Treatment of Pressure Ulcers/Injuries: International Guideline (4th ed.).
Oomens, C.W.J., et al. (2015). Biomechanics of deep tissue injury. Journal of Biomechanics, 48(12), 3386–3393.
Santamaria, N., et al. (2015). Clinical effectiveness of alternating pressure surfaces. Wound Repair and Regeneration, 23(3), 420–427.
